Pediatric Medical Billing Services

How To Choose The Best Pediatric Medical Billing Services?
In the dynamic world of healthcare, the importance of efficient and accurate medical billing services can’t be overstated. For pediatric practices, which focus on the health and well-being of children, having streamlined billing processes is even more crucial.
Pediatric medical billing services ensure healthcare providers can concentrate on what matters most: delivering exceptional care to young patients. These services handle the complexities of insurance claims, coding regulations, and reimbursement procedures, lifting the administrative burden from pediatric practices and allowing them to devote their full attention to nurturing children’s health and development.
Apex Medical Billing Company
When it comes to pediatric medical billing, you need a partner who understands the unique challenges and requirements of pediatric care.
Apex Medical Billing offers specialized services designed to meet the needs of pediatricians and pediatric subspecialists. By outsourcing your billing and coding tasks to our experts, you can save time, reduce errors, and increase your revenue.
Here are some of the benefits of choosing Apex Medical Billing:
- Comprehensive Billing and Coding Services: We handle a wide range of pediatric services, including vaccinations, preventive care, developmental screening, behavioral health, and chronic disease management.
- Compliance and Audits: We ensure your documentation meets all pediatric billing guidelines and requirements, reducing the risk of claim denials.
- Insurance Credentialing: Our team helps you enroll with various payers and negotiate favorable contracts with optimal fee schedules.
- Provider Education: We offer training to help you improve documentation techniques, ensuring higher codes are billed appropriately.
- Full Transparency and Reporting: Stay informed with detailed updates on claims, payments, denials, appeals, and collections.
- Customer Service: Our team handles patient calls about payments, billing questions, and payment plans.
Pediatrics Medical Credentialing Services
Pediatric medical credentialing is vital for verifying and validating the qualifications, skills, and competencies of pediatricians. The credentialing process includes:
- Educational and Professional Verification: Reviewing educational background, training, certifications, licenses, and work history.
- Performance Evaluation: Assessing clinical performance, outcomes, and competencies.
- Credential Maintenance: Regular updates on credentials and privileges to ensure compliance.

Pediatrics Prior Authorization Services
Navigating prior authorization can be a daunting task. Our services help pediatricians obtain necessary approvals from insurance companies for specific treatments or equipment. Here’s how we assist:
- Verification Services: Confirming the child’s eligibility, benefits, and coverage for requested services.
- Authorization Initiation: Submit prior authorization requests with all necessary clinical documentation.
- Authorization Follow-up: Tracking the status and resolving any issues or queries.
- Authorization Update: Keeping the pediatrician and the child’s family informed about the outcome.
- Authorization Renewal: Monitoring expiration dates and initiating renewal requests when needed.
Pediatrics CPT Codes
Pediatrics CPT codes describe the services and procedures performed by pediatricians. These codes are essential for billing, coding, reimbursement, and quality reporting. Key details include:
- Range of Codes: Covering various services such as preventive care, office visits, immunizations, developmental screening, behavioral health, and more.
- Specific Descriptions: Indicating the type, location, method, and duration of the service or procedure.
- Modifiers: Providing additional information such as laterality, multiple procedures, and more.
- Annual Updates: Reflecting changes in medical practice and technology.
Benefits Of Outsourcing Pediatrics Medical Billing
Outsourcing pediatric medical billing can transform your practice. Here are some of the advantages:
- Increased Revenue: Reduce billing errors, improve claims submission, and boost overall revenue.
- Reduced Errors: Minimize the risk of claim denials, rejections, or delays with accurate billing practices.
- Improved Cash Flow: Ensure prompt claim submission, accurate payment posting, and efficient accounts receivable management.
- Cost Savings: Lower overhead costs related to staff salaries, training, software, and hardware.
Why Choose Apex as Your Billing Partner?
Choosing Apex for your pediatric medical billing means opting for a partner dedicated to your success. Here’s why we stand out:
Certified and Experienced Team
Our specialists are well-versed in the latest pediatric coding and billing guidelines and standards.
Advanced Technology
Our secure billing software streamlines your process and reduces errors and denials.
Transparent Pricing
We offer flexible pricing plans with no hidden fees.
High Accuracy
We ensure 98% or above accuracy and clean claims on the first submission.
Increased Revenue
Proven track record of increasing client revenue by 30% or more.
24/7 Customer Support
Dedicated account managers ready to assist you at any time.
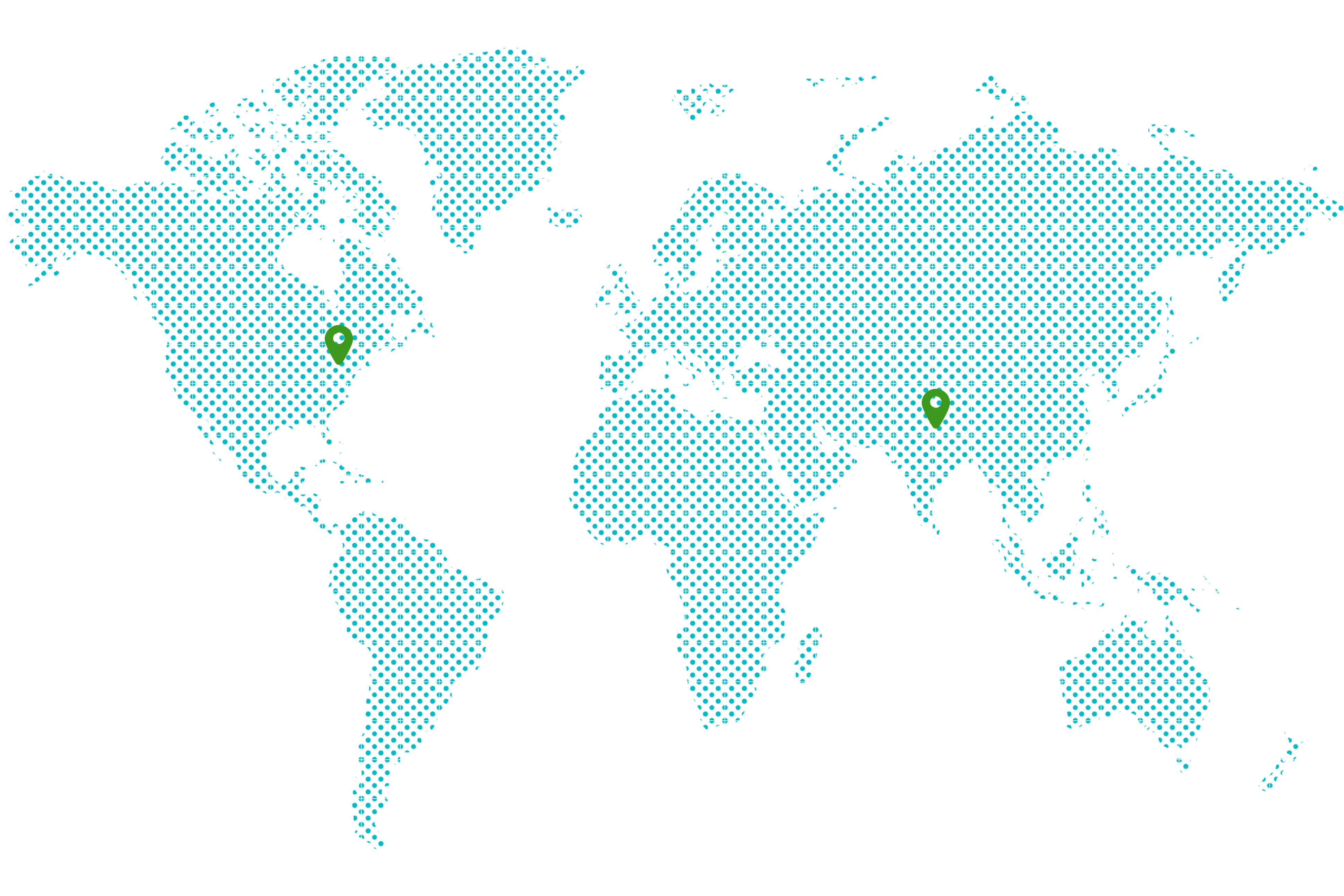
Support Area
Need help? Our expert team is here to assist you. Drop us a message and our support team will get back to you promptly.
Frequently Asked Questions
Pediatric medical billing involves creating and submitting insurance claims for services provided by pediatricians and pediatric subspecialists, ensuring accurate coding and timely reimbursement.
Key services include billing and coding, claims submission, insurance credentialing, compliance audits, and provider education.
Outsourcing can increase revenue, reduce billing errors, improve cash flow, and lower administrative costs, allowing you to focus more on patient care.
Credentialing includes verifying educational and professional qualifications, evaluating clinical performance, and maintaining updated credentials.
Prior authorization is the process of obtaining approval from insurance companies for specific treatments or equipment before they are provided to ensure coverage and reimbursement.